I always preach about the risk vs. the reward with this procedure. Each patient's risk vs. reward list will look a little different, and you have to put it together and decide to do what is best for you as the patient. Best place to start with this is knowing what the risks are. Just like any surgery, there are risks. I feel like there are a few more riskier risks with this procedure since you're 1.) this is super invasive and messing with your skull/face and other important areas, and 2.) you're messing with your teeth/jaw. You eat, breath, and speak using these bones, muscles, and teeth. Having them compromised would definitely be a drag on your quality of life.
That said, there are "typical" minor risks with this procedure. I guess compared to everything I've been through I would consider them minor, but before the surgery I did consider it a major risk and it was a huge pre op deal to me. First and foremost is the paraethesia. This is the numbness you hear everybody talking about on every fb group, message forum, or blog from here to timbuktu. The older you are, the greater chance you have to see a few permanent patches of tingly/numbness; more than likely across your bottom lip or chin if you are doing lower jaw surgery. The more invasive and/or more difficult your work, the greater chance of lingering numbness. The first few weeks out of surgery I was numb on my right half from my chin up to my lower eye lid. I was expecting the chin/lips, but I'll admit, the upper cheek and eye were a surprise and I didn't like it one bit. My left side was completely fine, so I am guessing my right side along the nerve got man handled at one point during surgery. I got feeling back in the upper cheek/eye within the first 3-4 weeks. It took a few months for more of my chin/lips to come back, but ultimately I was left with a strip of numbness across my right lower lip horizontally, and have a vertical a little strip along the right side of my chin. Most of my gums on the right side do not have full sensation back (and are in spots still numb), and there are a few little spots that are hyper sensitive. With revision I was almost guaranteed to lose more feeling, but I got extremely lucky and within the first 3 months post op, I had everything back up to that original patch of numbness from the first surgery. You'll hear people say that you get used to it and it really isn't a big deal, and for most cases, they're right. I'm totally used to mine and I can live with the numbness I have left. I don't really think about it unless I brush my chin and remind myself that it feels a little weird. There are a few cases of extreme issues though, like when somebody also loses some motor function and/or taste. From what I've read and heard about, these are pretty rare cases. Even when people have the nerve completely severed, they're usually just numb with no function loss. For me, the risk was worth the reward here. I was ready to pay the price of having a little numbness in return for having my bite issues fixed. My advice is to go in assuming you're going to have some numbness after. If you heal and get all of your feeling back, then think of it as a bonus!
Tooth damage. There can be some tooth damage with the surgery. I feel life more often than not, the most damage I've seen actually comes from the ortho side of this journey, but surgery can kill the roots of your teeth. They can slip with instruments and break teeth. Basically it comes down to the fact that something can happen and you can either end up having to have a root canal to save a tooth, or the tooth will be a goner all together in extreme cases. In my experience, most people see damage from ortho and the associated root resorption. That was my case. My upper 4 front teeth (both lateral incisors and main incisors) and 3 lower incisors have seen severe-extreme resorption and will need to be replaced and fully restored after treatment. In my case, this was probably a biological response and also a response to the overly aggressive movements my first ortho did with me.
Joint changes. Another thing with this surgery is there is no high confidence guarantee for what happens with your joints. If you're doing this to help your TMJ, they hope it will improve after surgery, but sometimes for whatever reason it doesn't. Or you could go in to surgery with zero joint issues, but come out with some. TMJ's are funny joints, and in my experience I've seen outcomes go all sorts of directions when it comes to them. In my own experience I feel like I had less problems with my joints before surgery than I do now post op, but that also could be because of what my joints had to go through sitting twisted for two years and having to endure two major jaw surgeries and go through two periods of remodeling. For all intents and purposes, even though they are worse than before, they are still in great shape given what I put them through the last 3 years.
I wanted to address a topic that most doctors do not talk about: Stroke. As with any surgery, there is a chance of stroke and clot. When I woke up from surgery I had these air cuffs around my legs that helped to circulate blood and prevent clots, which could lead to something like a stroke or pulmonary embolism. I wasn't expecting them, so it was just a surprise to wake up with them on my legs. My husband was intrigued too, and inquired about them and did some research while I was dozing in and out in my post op morphine haze. He read more on blood clot risks and found a lot of information regarding birth control and increased chance for clots and stroke. I went in to my surgery on birth control. A lot of women do, and most of the time everything is fine. I do know of one patient who unfortunately had a stroke in the hours immediately after surgery. Who knows if birth control was the direct cause of that, as strokes can happen off of birth control, but the fact is that it does increase your risk. Doctors do not do a good job of addressing this issue with female patients. My doc was a woman and I never heard a peep from her regarding this, although I am sure it was buried in the fine print that outlined my risks on a piece of paper I signed somewhere. My advice: get off of your birth control prior to surgery. I was even give it two cycles to get it out of your system. You've really got nothing to lose by doing this.
Another risk like any other surgery is the chance for an undesirable surgical outcome. This was a risk I thought about a lot prior to surgery. I looked for blogs where people were not happy, where the proverbial shit really did hit the fan, and tried to understand what that take on things were. I took that in to account in weighing the risks vs. the reward for me. Keep in mind that most people on internet forums are there because something didn't go right and they got online for help/support (not the case with me as I've been this vocal from day 1 before any shit hit any fan), so I took what people online said with a little more of a grain of salt and put more stock in blogs I found, especially those that were written by patients, unbiased, from day 1. From my research and experience with patients, this surgery has a high success rate in terms of catastrophic failure. Weighing that in to my risk vs. reward, I figured it was worth the risk and roll of the dice, hoping I stay in the majority of patients who turn out A-OK. Unfortunately, I did not end up in that majority, or close to it. Reading the blogs before hand prepared me for this scenario, and I am incredibly grateful that I went in to this surgery with a realistic/practical expectation, as well as a good understanding of risks like this one. I think the one area where this becomes a huge deal is when people do not walk in to this surgery with a practical outlook and/or realistic expectations. Or they approach it with the notion that something like this could never happen to them. It can, and all you can do is understand the risk and be prepared to deal with it if it unfortunately does happen to you. Another area that concerns me is patients, most of whom tend to be in the camp where they believe things can never go bad for this, walk in to this surgery hinging their whole well being and future life on this surgery. A lot of the patients I've come across in this camp are primarily doing this for cosmetic reasons. If you fall in that category, please understand that 1.) You may see little to no change from this surgery. Surgeons are here to primarily fix functional issues, and functional outcomes they can better predict with better confidence. Soft tissue changes are VERY hard to predict and they can end up being totally subjective. Even more problematic here is some surgeons really sell patients the idea that they are going to look like a Hollywood diva when they're done with this surgery. IMO, they are doing the patients a huge disservice here. 2.) Not only could you see little to no changes, but you could end much worse than what you went in to fix. This unfortunately was my case, both aesthetically and functionally after my first surgery. Even though I was very realistic and practical about my expectations, this was still incredibly difficult to deal with. I can not imagine dealing with it if I had went in to this surgery with the notion that it was going to fix my life, make me automatically whole, and be an ultimate fix all. A person expecting that would have been completely shattered after, and god forbid, maybe even suicidal in my shoes post op. Hope for the best, prepare for the worst. Please understand that this may not be your ultimate fix all, even if it all goes right. It's best to keep an open mind and have realistic expectations.
Another issue I experienced post op and would probably put it under the minor risks associated with this procedure is hair loss. This was also something I read about pre op and was on my toes for. Immediately post op I had no issues, but at 3 months post, BAM!! Hair is falling out like crazy. My brush was as full daily as it used to be over a few weeks. I never lost hair in clumps where I had stark bald spots, but it was more of an overall uniform falling out and thinning. My crown around my forehead and temples got really thin and bald looking in a few spots. I've come across a few other patients who said it was around the 3 month mark that they experienced issues too. From what I've researched, this is a similar problem that bariatric patients experience, or sometimes pregnant and/or postpartum mothers. The hair follicles get thrown out of their mojo. They get shocked, fall out, and then get stuck in this phase where they are stagnant for a bit, and then (hopefully), you see regrowth. What does the shocking for a jaw surgery patient? Some say lengthy general anesthesia can mess some people up and throw your system out of whack. We also go through a period where the body experiences immediate major trauma with our faces being broken in to multiple pieces. All of our energy is going towards healing, and energy is something we have little fuel for since our diets are drastically modified. In my case, I wasn't getting more than 300-600 calories per day for the first month after surgery. Maybe 1000 calories max after I was able to start soft chew 2 weeks post op. Just going from eating what you want to nothing is a shock to the body, let alone doing that when it needs all the energy it can to heal all of the facial trauma you just went through. I took a multi vitamin, fish oil, biotin, hair/skin/nails gummy vitamin, probiotic, tumeric, and started using expensive Nioxin shampoo. The nioxin and biotin made a difference, and I was later eating a pretty healthy mostly whole foods diet, but in the end I think this shock in our follicle cycle just takes time. My hair has finally stopped falling out and returned to a more normal loss rate around 10 months post op. I now have a lot of baby hairs and fly aways present as things fill back in.
********
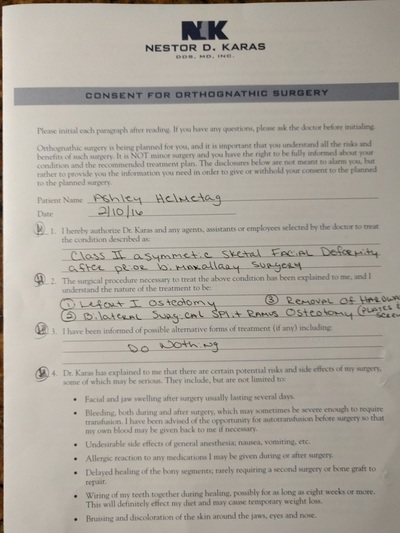
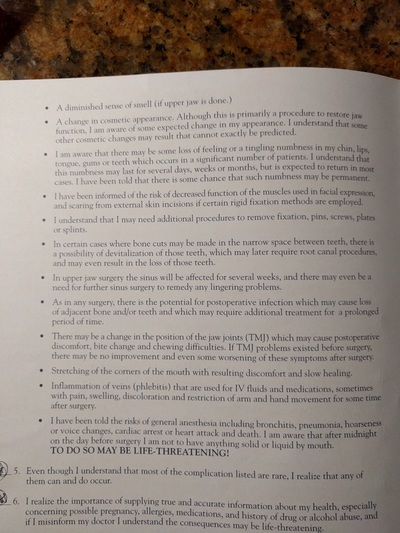
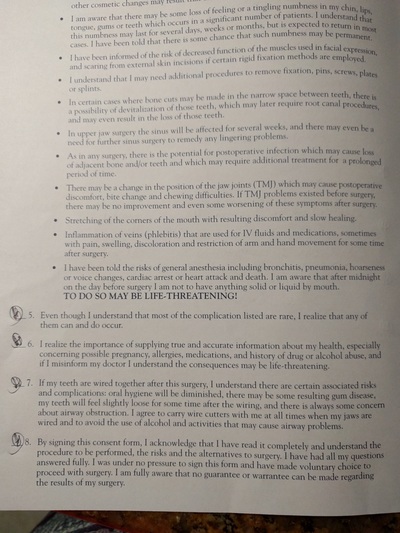
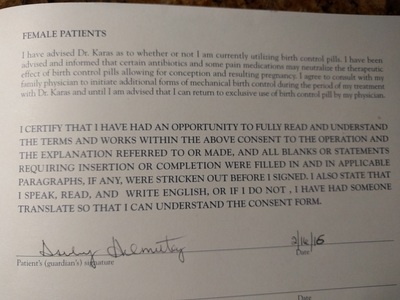
Update after revision surgery. I wanted to update a little section devoted to my revision surgeons risks/consent form. I thought it was great! Covered much more than my Kaiser forms, and compared to other forms or consent I've seen patients talk about online, it seems to do better too. I didn't get a chance to scan it in before having to give back to my doc prior to surgery, but I was able to snap a few pictures with my phone. Check it out. I think he did a good job of covering even the less talked about risks like birth control not working as well on antibiotic and soft tissue changes that can not be predicted.
That said, there are "typical" minor risks with this procedure. I guess compared to everything I've been through I would consider them minor, but before the surgery I did consider it a major risk and it was a huge pre op deal to me. First and foremost is the paraethesia. This is the numbness you hear everybody talking about on every fb group, message forum, or blog from here to timbuktu. The older you are, the greater chance you have to see a few permanent patches of tingly/numbness; more than likely across your bottom lip or chin if you are doing lower jaw surgery. The more invasive and/or more difficult your work, the greater chance of lingering numbness. The first few weeks out of surgery I was numb on my right half from my chin up to my lower eye lid. I was expecting the chin/lips, but I'll admit, the upper cheek and eye were a surprise and I didn't like it one bit. My left side was completely fine, so I am guessing my right side along the nerve got man handled at one point during surgery. I got feeling back in the upper cheek/eye within the first 3-4 weeks. It took a few months for more of my chin/lips to come back, but ultimately I was left with a strip of numbness across my right lower lip horizontally, and have a vertical a little strip along the right side of my chin. Most of my gums on the right side do not have full sensation back (and are in spots still numb), and there are a few little spots that are hyper sensitive. With revision I was almost guaranteed to lose more feeling, but I got extremely lucky and within the first 3 months post op, I had everything back up to that original patch of numbness from the first surgery. You'll hear people say that you get used to it and it really isn't a big deal, and for most cases, they're right. I'm totally used to mine and I can live with the numbness I have left. I don't really think about it unless I brush my chin and remind myself that it feels a little weird. There are a few cases of extreme issues though, like when somebody also loses some motor function and/or taste. From what I've read and heard about, these are pretty rare cases. Even when people have the nerve completely severed, they're usually just numb with no function loss. For me, the risk was worth the reward here. I was ready to pay the price of having a little numbness in return for having my bite issues fixed. My advice is to go in assuming you're going to have some numbness after. If you heal and get all of your feeling back, then think of it as a bonus!
Tooth damage. There can be some tooth damage with the surgery. I feel life more often than not, the most damage I've seen actually comes from the ortho side of this journey, but surgery can kill the roots of your teeth. They can slip with instruments and break teeth. Basically it comes down to the fact that something can happen and you can either end up having to have a root canal to save a tooth, or the tooth will be a goner all together in extreme cases. In my experience, most people see damage from ortho and the associated root resorption. That was my case. My upper 4 front teeth (both lateral incisors and main incisors) and 3 lower incisors have seen severe-extreme resorption and will need to be replaced and fully restored after treatment. In my case, this was probably a biological response and also a response to the overly aggressive movements my first ortho did with me.
Joint changes. Another thing with this surgery is there is no high confidence guarantee for what happens with your joints. If you're doing this to help your TMJ, they hope it will improve after surgery, but sometimes for whatever reason it doesn't. Or you could go in to surgery with zero joint issues, but come out with some. TMJ's are funny joints, and in my experience I've seen outcomes go all sorts of directions when it comes to them. In my own experience I feel like I had less problems with my joints before surgery than I do now post op, but that also could be because of what my joints had to go through sitting twisted for two years and having to endure two major jaw surgeries and go through two periods of remodeling. For all intents and purposes, even though they are worse than before, they are still in great shape given what I put them through the last 3 years.
I wanted to address a topic that most doctors do not talk about: Stroke. As with any surgery, there is a chance of stroke and clot. When I woke up from surgery I had these air cuffs around my legs that helped to circulate blood and prevent clots, which could lead to something like a stroke or pulmonary embolism. I wasn't expecting them, so it was just a surprise to wake up with them on my legs. My husband was intrigued too, and inquired about them and did some research while I was dozing in and out in my post op morphine haze. He read more on blood clot risks and found a lot of information regarding birth control and increased chance for clots and stroke. I went in to my surgery on birth control. A lot of women do, and most of the time everything is fine. I do know of one patient who unfortunately had a stroke in the hours immediately after surgery. Who knows if birth control was the direct cause of that, as strokes can happen off of birth control, but the fact is that it does increase your risk. Doctors do not do a good job of addressing this issue with female patients. My doc was a woman and I never heard a peep from her regarding this, although I am sure it was buried in the fine print that outlined my risks on a piece of paper I signed somewhere. My advice: get off of your birth control prior to surgery. I was even give it two cycles to get it out of your system. You've really got nothing to lose by doing this.
Another risk like any other surgery is the chance for an undesirable surgical outcome. This was a risk I thought about a lot prior to surgery. I looked for blogs where people were not happy, where the proverbial shit really did hit the fan, and tried to understand what that take on things were. I took that in to account in weighing the risks vs. the reward for me. Keep in mind that most people on internet forums are there because something didn't go right and they got online for help/support (not the case with me as I've been this vocal from day 1 before any shit hit any fan), so I took what people online said with a little more of a grain of salt and put more stock in blogs I found, especially those that were written by patients, unbiased, from day 1. From my research and experience with patients, this surgery has a high success rate in terms of catastrophic failure. Weighing that in to my risk vs. reward, I figured it was worth the risk and roll of the dice, hoping I stay in the majority of patients who turn out A-OK. Unfortunately, I did not end up in that majority, or close to it. Reading the blogs before hand prepared me for this scenario, and I am incredibly grateful that I went in to this surgery with a realistic/practical expectation, as well as a good understanding of risks like this one. I think the one area where this becomes a huge deal is when people do not walk in to this surgery with a practical outlook and/or realistic expectations. Or they approach it with the notion that something like this could never happen to them. It can, and all you can do is understand the risk and be prepared to deal with it if it unfortunately does happen to you. Another area that concerns me is patients, most of whom tend to be in the camp where they believe things can never go bad for this, walk in to this surgery hinging their whole well being and future life on this surgery. A lot of the patients I've come across in this camp are primarily doing this for cosmetic reasons. If you fall in that category, please understand that 1.) You may see little to no change from this surgery. Surgeons are here to primarily fix functional issues, and functional outcomes they can better predict with better confidence. Soft tissue changes are VERY hard to predict and they can end up being totally subjective. Even more problematic here is some surgeons really sell patients the idea that they are going to look like a Hollywood diva when they're done with this surgery. IMO, they are doing the patients a huge disservice here. 2.) Not only could you see little to no changes, but you could end much worse than what you went in to fix. This unfortunately was my case, both aesthetically and functionally after my first surgery. Even though I was very realistic and practical about my expectations, this was still incredibly difficult to deal with. I can not imagine dealing with it if I had went in to this surgery with the notion that it was going to fix my life, make me automatically whole, and be an ultimate fix all. A person expecting that would have been completely shattered after, and god forbid, maybe even suicidal in my shoes post op. Hope for the best, prepare for the worst. Please understand that this may not be your ultimate fix all, even if it all goes right. It's best to keep an open mind and have realistic expectations.
Another issue I experienced post op and would probably put it under the minor risks associated with this procedure is hair loss. This was also something I read about pre op and was on my toes for. Immediately post op I had no issues, but at 3 months post, BAM!! Hair is falling out like crazy. My brush was as full daily as it used to be over a few weeks. I never lost hair in clumps where I had stark bald spots, but it was more of an overall uniform falling out and thinning. My crown around my forehead and temples got really thin and bald looking in a few spots. I've come across a few other patients who said it was around the 3 month mark that they experienced issues too. From what I've researched, this is a similar problem that bariatric patients experience, or sometimes pregnant and/or postpartum mothers. The hair follicles get thrown out of their mojo. They get shocked, fall out, and then get stuck in this phase where they are stagnant for a bit, and then (hopefully), you see regrowth. What does the shocking for a jaw surgery patient? Some say lengthy general anesthesia can mess some people up and throw your system out of whack. We also go through a period where the body experiences immediate major trauma with our faces being broken in to multiple pieces. All of our energy is going towards healing, and energy is something we have little fuel for since our diets are drastically modified. In my case, I wasn't getting more than 300-600 calories per day for the first month after surgery. Maybe 1000 calories max after I was able to start soft chew 2 weeks post op. Just going from eating what you want to nothing is a shock to the body, let alone doing that when it needs all the energy it can to heal all of the facial trauma you just went through. I took a multi vitamin, fish oil, biotin, hair/skin/nails gummy vitamin, probiotic, tumeric, and started using expensive Nioxin shampoo. The nioxin and biotin made a difference, and I was later eating a pretty healthy mostly whole foods diet, but in the end I think this shock in our follicle cycle just takes time. My hair has finally stopped falling out and returned to a more normal loss rate around 10 months post op. I now have a lot of baby hairs and fly aways present as things fill back in.
********
Update after revision surgery. I wanted to update a little section devoted to my revision surgeons risks/consent form. I thought it was great! Covered much more than my Kaiser forms, and compared to other forms or consent I've seen patients talk about online, it seems to do better too. I didn't get a chance to scan it in before having to give back to my doc prior to surgery, but I was able to snap a few pictures with my phone. Check it out. I think he did a good job of covering even the less talked about risks like birth control not working as well on antibiotic and soft tissue changes that can not be predicted.